 One of the most important considerations in managing type 2 diabetes is making appropriate diet choices, anything that you eat needs to be considered in terms of blood sugar impact. Nutrition therapy is key, as it is food that causes blood sugar spikes and greatly influences blood glucose levels. It is possible to keep those glucose levels stable, and it all begins with meal planning.
One of the most important considerations in managing type 2 diabetes is making appropriate diet choices, anything that you eat needs to be considered in terms of blood sugar impact. Nutrition therapy is key, as it is food that causes blood sugar spikes and greatly influences blood glucose levels. It is possible to keep those glucose levels stable, and it all begins with meal planning.
Goals of Nutrition Therapy
The serious complications associated with Type 2 diabetes can be avoided with careful blood sugar management, diet, exercise and weight loss (if needed). Careful monitoring of blood sugars and the condition in general by a medical professional is important since out of control blood sugars can lead to diabetic coma, along with all the other complications.
According to the American Diabetes Association, the goal of any sound nutritional plan for diabetes is to support and promote healthy eating, with a diet plan that includes a variety of nutrient dense foods in appropriate portion sizes.
Goals of Nutritional Therapy:
- Reduce the hemoglobin A1C test to less than 7%
- Maintain healthy blood pressure.
- Maintain healthy cholesterol levels.
- Maintain a healthy weight.
- Delay or prevent any possible complications of diabetes.
- Create a personalized diet plan that meets the individual’s personal and cultural circumstances and one that considers the patient’s access to healthy food, and their willingness to make lifestyle changes or else address any barriers to make such changes.
- Enjoy variety in diet and include restrictions only when they are backed by scientific evidence.
- Focus on practical day-to-day meal planning instead of complicated counting of nutrients, carbs, or particular foods.
The Diabetic Plate
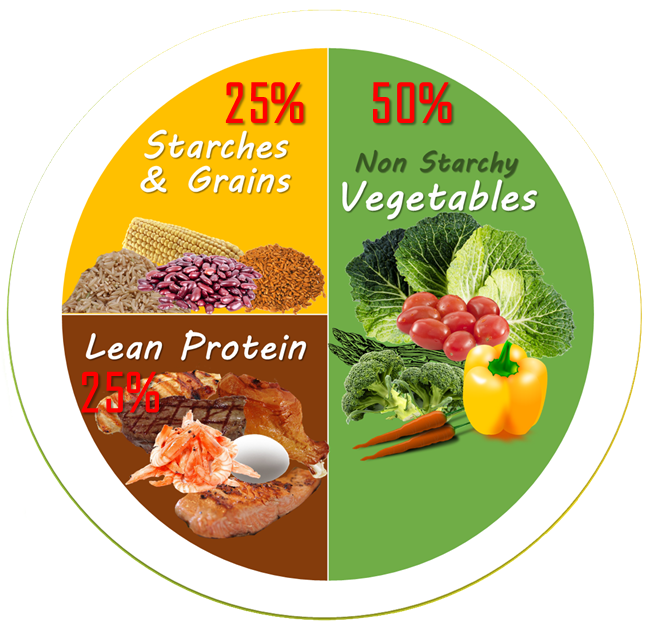
The American Diabetes Association takes a no-nonsense view of the proper diet for diabetics. Instead of complicated counting of calories, carbs, or the need for special tools, they use the diabetic plate model that creates a simple method of healthy eating that is accessible to anyone to control their diabetes.
As you can see, the diabetic plate is a simple method that only requires you to divide the plate into sections and fill it with the appropriate foods.
This simplifies the process for everyone. There are liberal food choices, and since the choices are all healthy, this method allows diabetics to enjoy the same meals as the rest of the family without having to do special shopping or preparation. The aspect of choice with using the plate method surpasses barriers that might otherwise prevent diabetics from eating an appropriate diet. Let’s take a closer look at the plate.
Non Starchy Vegetables
50% of the entire plate should be filled with non-starchy vegetables, which include:
- All Greens, Kale and Spinach
- Carrots
- Mushrooms
- Cucumbers
- Tomatoes
- Onions
- Broccoli
- Cauliflower
- Peppers
- Green beans
- Beets
- Okra
- Mushrooms
- Turnips
- And others
Note: The more color you have on the vegetable section of your plate the wider the variety of nutrients you take in.
Starches and Grains
25% of the plate should be filled with grains and starches. This includes:
- Corn
- Sweet Potatoes
- Peas
- Beans
- Oatmeal
- Whole grains: rice, pasta, bread and cereals
Choose whole grains over processed white varieties, including pasta, rice, and bread. Whole grains are not stripped of vital nutrients like their white counterparts and they are high fiber, an essential nutrient for managing blood sugar. Fiber in food allows blood sugars to increase gradually during and after eating, as opposed to radical spikes.
Repeated studies document that whole grains can prevent the onset of type 2 diabetes by 21% to 30% and they go a long way to helping those diagnosed with either type 2 diabetes or prediabetes maintain low blood glucose levels.
Lean Protein
The final section of the plate is for lean protein, which includes:
- Beef
- Chicken
- Fish
- Seafood
- Eggs
- Tofu
- Pork
- Low Fat Cheese
Since diabetics are at a higher risk for heart disease, it is important to consider fat intake in the diet. Animal protein is typically higher in saturated fat than other protein choices and therefore can make more of an impact on heart health.
Limit high fat meats or processed meats. They can only raise your cholesterol levels, making complications of diabetes more likely. Lean turkey meat, and white skinless chicken contain less saturated fats and are quality protein choices.
All fish is a wonderful option, and especially, fatty fish that provides healthy omega-3 fatty acids and is found in herring, trout, sardines, albacore tuna, and salmon.
Healthy Fats
Healthy fats in moderation, including monosaturated and polyunsaturated should be included in any diet, including that for type 2 diabetes because they greatly contribute to heart health. Healthy fats come in two forms:
Monosaturated Fat Foods
- Olive oil, coconut oil
- Avocados
- Peanut butter
- Many nuts and seeds
Polyunsaturated Fat Foods
Omega-6 Fatty Acids Sources:
- Walnuts and seeds
Omega-3 Fatty Acids Sources:
- Salmon, herring, Albacore tuna, rainbow trout, mackerel and sardines
- Walnuts
- Flaxseed
- Beef
- Tofu
- Shrimp
- Brussels Sprouts
- Cauliflower
The American Heart Association recommends that saturated fats should be limited to 7% or less of one’s daily caloric intake. Trans fats should be kept to 1% or less, as they are the most harmful for the heart. Heart disease is of special concern for those with diabetes because they are at higher risk for it, therefore eating healthy fats and limiting unhealthy varieties is of utmost importance.
Carbohydrates
The main concern in a diabetes friendly diet is carbohydrates as they make the most impact on blood sugars.
Carbohydrates are biomolecules or saccharides that play significant roles in the human body, including providing it with energy, support in fertilization, immune system functions, blood clotting, and development.
In simple terms, carbohydrates are sugars.
All plant-based foods contain some form of carbohydrates but whileall starches are carbohydrates, not all carbohydrates are starches.
All simple sugars and starches are converted to glucose in the body (the only exceptions are sugar alcohols and insoluble fiber), the main difference is the speed with which this occurs, and that is what is most important as far as type 2 diabetes is concerned. There are two main forms of carbohydrates
Simple Carbohydrates
Simple carbohydrates are simple sugars made up of only one or two sugar (saccharide) chains. This category includes fast acting carbohydrate sugars and starches. Simple carbs are digested very quickly by the body and therefore cause sudden floods of glucose into the blood stream.
Simple Carbohydrates Include: table sugar, candy, soda, fruit, honey, syrup, and juices.
Complex Carbohydrates
Complex carbohydrates are starches and are comprised of thousands of sugar chains. Complex carbs are digested slowly by the body, which incur gradual rises in blood glucose levels.
Complex Carbohydrates Include: starchy vegetables like corn and peas, along with potatoes, beans, rice, cereals and grains and fiber.
The main difference between simple and complex carbs is how they are digested and absorbed in the body along with chemical structure.
The Role of Fiber
Those with impaired glucose tolerance and insulin resistance have a higher risk for cardiovascular disease because increased blood glucose and insulin concentrations are associated with high cholesterol (LDL) and decreased good (HDL) cholesterol, both of which are risk factors for cardiovascular disease.
- Fiber helps to lower bad cholesterol and prevent heart disease.
- Fiber helps to lessen the impact of carbohydrates on blood glucose levels. Soluble fiber especially, delays the absorption of nutrients in the body and therefore slows the rise of blood sugars after a meal.
- Fiber is the reason that whole grains are recommended over processed grains because the processing strips the grain of fiber, leaving higher impact carbs.
- Fiber is also the reason whole fruit is recommended over juicing because the juicing process removes the pulp of the fruit where the fiber lies, and therefore makes juice higher in sugar impact carbs than eating the whole fruit.
The more fiber a food has, the less impact it will have on blood sugars.
Fiber Rich Foods:
- Fresh fruits and vegetables and especially green and leafy green varieties
- Nuts and seeds
- Dried beans and peas
- Whole Grains: bread, wild rice, whole grain flours, and crackers
- Brown rice and wild rice
Non-starchy vegetables that are high in fiber and low in calories are some of the best sources of fiber.
Whole grains “brown” starches are much better choices than their “white” processed counterparts that have a much lower fiber content.
Note: While whole grains provide valuable nutrients, they still have more impact on blood glucose than vegetable carbs, and so portion size should always be considered.
Assessing the Impact of Carbohydrates
While in the past carbohydrate considerations were mainly based on the classifications of simple versus complex, this method has proved to be much too simplistic because the blood glucose (glycemic) response to complex carbohydrates has been found to vary considerably.
Glycemic load has been deemed a more accurate indicator of blood glucose impact from dietary carbohydrates, which in addition to the food itself also incorporates considerations as to the relative quality and quantity of carbohydrates in the diet.
The Glycemic Index
Glycemic load is assessed by the Glycemic Index (GI), and is another method to help control blood glucose by choosing foods with low GI scores.
The glycemic index is a scale that ranks food on a scale of 0 to 100 based on the impact they have in raising blood sugar levels after eating.
Foods that have a moderate to high GI score digest quickly and therefore cause blood sugar spikes. Conversely, low-GI foods digest slowly and incur gradual rises in sugar and insulin levels in the blood, an essential consideration for those with diabetes.
Factors that Influence Glycemic Load
- One of the factors in assessing glycemic load is the level at which a food is processed, typically the more processed a food, the higher the GI score. For example, one whole peach has a GI of 42, while a fruit roll up has a GI of 99. Instant oatmeal has a higher GI than steel cut oats.
- Certain combinations of carbs can influence glycemic load, as is the case when a high GI food is eaten with a lower one where the lower one can help to counteract the effects of the other.
- Cooking times make a difference because cooking further breaks down starches, which causes them to digest faster.
- Acidity makes a difference where pickling can lower the GI of a food. Sourdough bread contains an acid that make it lower on the GI scale than white bread.
- The naturally occurring coat on food makes a difference in glycemic load, such as the case in beans, seeds, and plant cell walls found on whole grains that act as a physical barrier to slow digestion as the carbs are broken down in the stomach. This is one of the reasons that whole grain foods have a lower GI than processed ones where that coat is removed.
What Science Says About Low GI Diets in Diabetes
Several large studies report that a diet high on the GI scale is associated with an increased risk of developing type 2 diabetes. However, the many studies conducted into a “low GI diet” for diabetes have yielded mixed results.
The Pros and Cons of GI
There are many commercial diets based on the GI index and, it can be helpful as part of the overall food choice decision-making process for those with type 2 diabetes. However, concerns exist as to its efficiency in using it as the sole method of dietary choices for those with type 2 diabetes.
The American Diabetes Association’s standards of care recommend the use of the glycemic index but only as a small part of the overall carbohydrate equation, and they take the position that GI only has a modest additional benefit for glycemic control, versus that observed when total carbohydrate intake is considered on its own.
This opinion and others are concerned with managing blood glucose by solely using the Glycemic Index, without other important considerations.
Many experts agree that a low GI should not be used in isolation, especially in those who want to lose weight as part of the goal of managing blood sugar. Other factors still need to be considered including, calorie control, lean protein, vitamins, and minerals, monitoring fat intake, fiber, and other essential nutrients.






